Before delving into the specifics of the Ulcerative Colitis diet plan, it's essential to have a basic understanding of Ulcerative Colitis. UC is a chronic inflammatory bowel disease that primarily affects the large intestine (colon) and the rectum. It causes inflammation, ulcers, and discomfort, leading to symptoms such as abdominal pain, diarrhoea, weight loss, and fatigue. For people who have ulcerative colitis, managing flare-ups and symptoms often involves avoiding trigger foods like alcohol and spicy dishes. Low-fibre fruits and vegetables can be added to the Ulcerative colitis diet plan to help reduce symptom exacerbation during flare-ups. Due to the fact that ulcerative colitis is a chronic inflammatory bowel illness, choosing the right Ulcerative colitis diet plan usually entails a process of elimination. People can create a customised diet that works for them by identifying and avoiding foods that aggravate symptoms.
Having a well-thought-out strategy in place can help some people manage their illness and reduce symptoms, even though there is no one diet that works best for everyone with ulcerative colitis. An individualised food plan can significantly enhance the general quality of life for those with ulcerative colitis. In this article, we will explore the key elements of an Ulcerative colitis diet plan and how it can positively impact the lives of those with this inflammatory bowel disease.
Meal Planning and Preparation:
Because there is currently no treatment for ulcerative colitis (UC), meal planning and preparation are essential for controlling the condition's symptoms. People with UC can successfully limit their intake of items that aggravate their symptoms by organising their meals and snacks in advance.
By planning ahead, you can avoid making quick choices that might trigger flare-ups and take control of what you eat and drink. It might save a lot of time throughout the week to set aside a few hours at the beginning of the week to prepare meals and examine nutrition labels. Buying ingredients in bulk, cooking in batches, and portioning meals for simple storage and reheating are helpful strategies.
Preparing meals ahead of time not only saves time, but it also helps to reduce food triggers, improving overall well-being and productivity. Planning snacks beforehand might also help prevent reaching for foods that might aggravate UC symptoms.
Dietary requirements may vary for people who experience constipation as a symptom, therefore, individualised planning might be helpful. Additionally, it's crucial to plan water consumption given the frequent diarrhoea associated with UC to prevent dehydration and maintain adequate hydration levels. For those with UC, a well-planned food and hydration schedule can help with better symptom control and overall quality of life.
Maintaining a Food Journal: Keeping a food record can be extremely helpful in identifying specific triggers for UC since trigger foods might differ from person to person. Your doctor and you can more accurately identify particular food triggers and more effectively treat your UC symptoms by keeping a daily food journal and keeping track of when you experience digestive problems. This routine is very helpful when experimenting with new foods to determine how they affect your condition.
Eating while in Remission: Despite the fact that there is no treatment for UC, there may be times when symptoms temporarily go away. It's important to maintain a varied, nutrient-rich diet free of trigger foods during these times. Following successful diets that have helped other people with UC can extend the time spent in remission. To encourage general well-being, introduce new foods gradually and place a high priority on remaining hydrated.
It can help you feel good and stay hydrated during remission to include fibre-rich foods like oats, beans, and nuts, healthy fats like olive oil and nut and seed butter, as well as protein from lean meats, fish, and eggs. Your overall health can also be supported during these times by including whole grains in your Ulcerative colitis diet plan, such as whole wheat bread, pasta, and brown rice. Additionally, vitamin D supplements might be advantageous, but you must speak with your doctor before beginning any supplementation.
Read to know: Top Exercise Remedies for Arthritis Knee Pain
Ideal Foods Rich in Nutrients for Ulcerative Colitis:
Prioritising nutrient-rich foods is necessary for people with ulcerative colitis to achieve their dietary needs. Some good cuisine selections include the following:
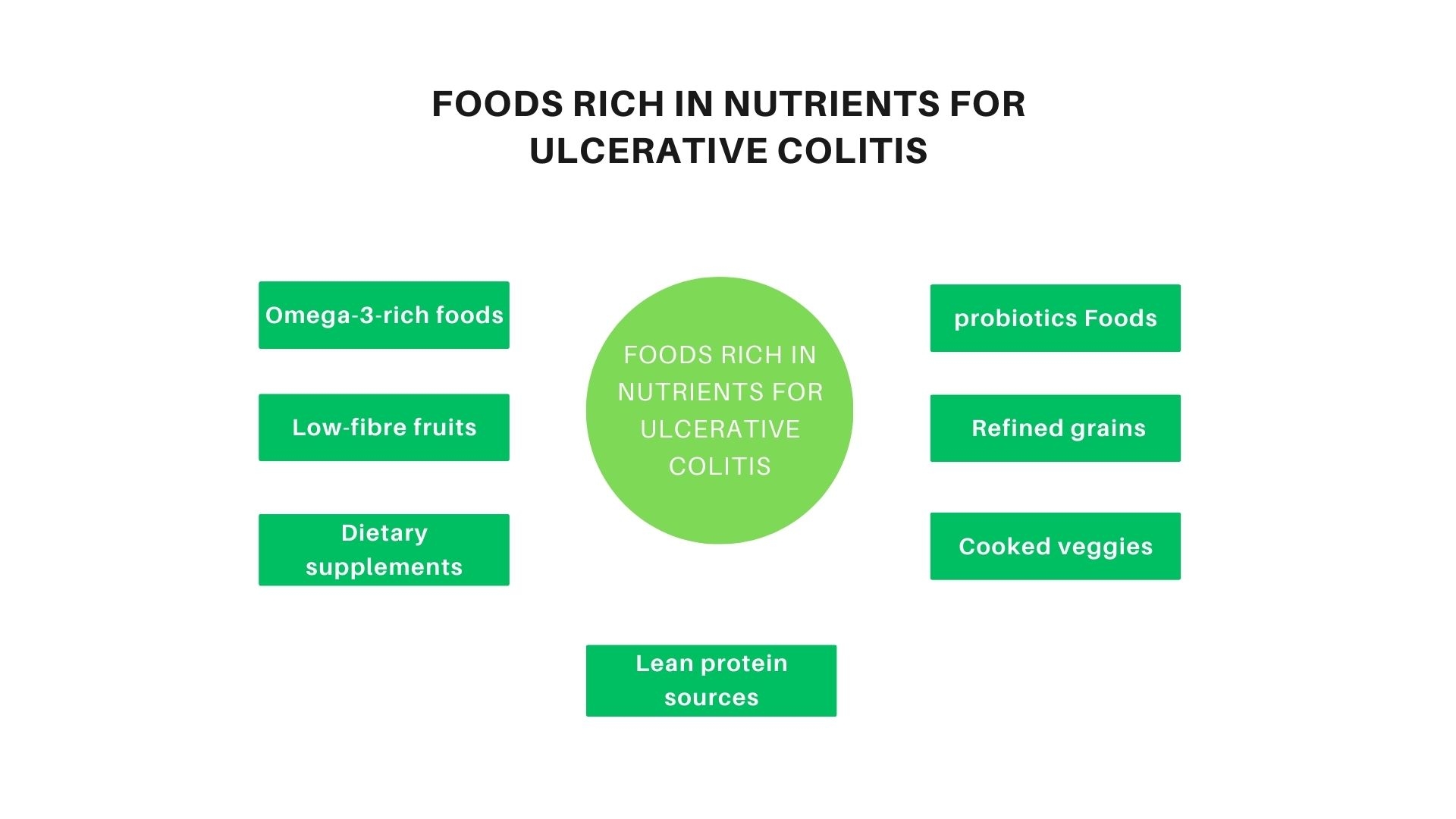
Omega-3-rich foods:
Include walnuts, flaxseed, hemp, salmon, mackerel, and chia seeds in your Ulcerative colitis diet plan. The International Organization for the Study of Inflammatory Bowel Diseases (IOIBD) suggests eating foods high in omega-3 fatty acids because of their possible health advantages in treating ulcerative colitis.
Foods containing probiotics:
Include probiotic-rich yoghurt in your Ulcerative colitis diet plan. These foods' healthy bacteria can improve digestion and possibly lessen ulcerative colitis flare-ups and symptoms.
Low-fibre fruits:
To prevent aggravating symptoms, choose readily digestible fruits like bananas, cantaloupes, and cooked fruits.
Refined grains:
Opt for readily digestible refined grains such as enriched oatmeal, white rice, gluten-free bread, and white pasta. These fortified goods offer important vitamins and minerals.
Lean protein sources:
Include fish, chicken, eggs, and firm tofu as lean protein sources; stay away from red meat.
Cooked veggies:
Non Cruciferous vegetables, such as cucumbers, squash, and asparagus tips, can be eaten without the skin and are often well accepted.
Dietary supplements:
Before using protein shakes or oral vitamin supplements, seek medical advice. These supplements may help ensure an appropriate nutrient intake, but it is still important to seek professional advice.
Foods to Avoid with Ulcerative Colitis:
Lactose products:
For some people, dairy products, including milk, cheese, and yogurt, might cause symptoms.
Red meat and processed meats:
Limit intake to avoid worsening symptoms.
Alcohol:
Alcoholic beverages may exacerbate the symptoms of ulcerative colitis.
Carbonated beverages: Some carbonated sodas and beers might irritate the digestive system.
Non Absorbable sugars:
Avoid artificial sweeteners and certain fruits like prunes, pears, and peaches.
Insoluble fibre foods:
Foods high in insoluble fibre should be avoided, especially whole grains, entire nuts, and fruits with peel.
Sugary foods:
Cakes, pastries, candies, and drinks all contain sugar and may cause flare-ups.
High-fat foods:
Avoid butter, fatty meats, coconut, and fried or greasy foods, as they are high in fat.
Foods that are spicy:
Hot sauces, chilies, and hot peppers might make symptoms worse.
Gluten:
Wheat, rye, and barley all contain the protein gluten, which some people with ulcerative colitis may find problematic.
Dietary emulsifiers:
Emulsifiers included in processed foods, such as carboxymethylcellulose and polysorbate-80, should be consumed in moderation.
You may also like to read, Remedies For Weight Loss
Conclusion:
While Ulcerative colitis diet plan cannot cure UC, it plays a crucial role in managing symptoms and reducing inflammation. A well-planned diet can help alleviate discomfort, prevent flare-ups, and promote gut healing. You can better control ulcerative colitis and promote your general health and well-being by including these nutrient-rich food options in your diet. In order to create a customised nutrition plan that addresses your unique condition and demands, don't forget to see a healthcare practitioner. A well-balanced Ulcerative colitis diet plan that includes appropriate proportions of macronutrients (carbohydrates, proteins, and fats) is essential for overall health. Consulting with a dietitian can help create a personalised meal plan that meets individual needs.
You may also like to read, 10 Best Foods to Boost Immunity